By Abdulkareem Haruna
A severe and rapidly expanding diphtheria outbreak is gripping northern Nigeria, overwhelming health facilities and exposing critical gaps in the region’s medical response.
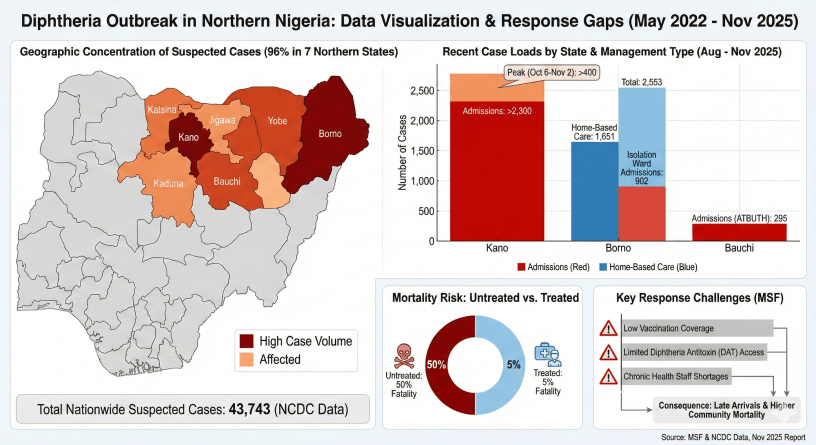
New data from Médecins Sans Frontières (MSF) and the Nigeria Centre for Disease Control (NCDC) reveals a dramatic surge in cases since August 2025, with the crisis concentrated almost exclusively in seven northern states.
According to the data, 96 percent of the 43,743 suspected cases reported nationwide between May 2022 and November 2025 have occurred in this region. The states of Kano and Borno are the hardest hit, marked by deep red on outbreak maps indicating the highest case volumes.
The situation has deteriorated sharply in the last few months. In Kano State, hospital admissions soared to over 2,300 between August and November 2025. The intensity of transmission was particularly acute during a four-week window from early October to early November, when more than 400 patients were admitted.
Borno State is also facing a massive caseload, with 2,553 recent cases reported. The strain on facilities has forced a reliance on home-based care for 1,651 patients, while 902 with more severe symptoms have been admitted to isolation wards. Bauchi State has also seen a significant rise, with 295 admissions recorded at a single teaching hospital.
The data highlights a stark and deadly reality for those infected. Diphtheria, a vaccine-preventable disease, carries a staggering 50 percent fatality rate if left untreated. However, with timely medical intervention, that risk plummets to just 5 percent. This tenfold difference underscores the critical urgency of getting patients to rapid and effective care.
Health officials are battling a perfect storm of challenges that are hampering the response and driving up mortality. MSF has identified three primary barriers: persistently low vaccination coverage in the affected areas, extremely limited access to the lifesaving Diphtheria Antitoxin (DAT), and chronic shortages of qualified health staff.
The consequence of these systemic failures is a tragic pattern of late arrivals at treatment centers, resulting in a higher number of preventable deaths within communities. The data paints a clear picture of a public health crisis where the difference between life and death hinges on resources that are currently in desperately short supply.